Optimising Breast Ultrasound Image Quality: Impact of Body Mass Index on Breast Carcinoma Detection on Women
DOI:
https://doi.org/10.37934/sijphpc.4.1.4051Keywords:
Breast carcinoma, Body Mass Index (BMI), ultrasound imaging, image quality, breast cancer detection, spatial resolution, contrast resolution, diagnostic imagingAbstract
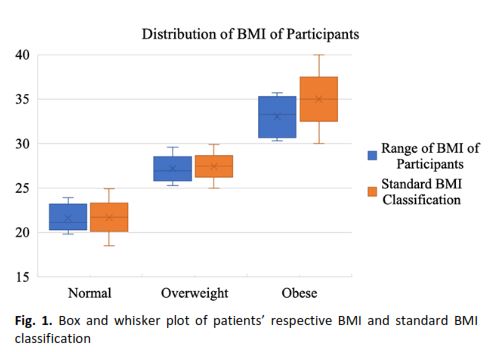
Breast carcinoma remains a leading cause of cancer-related mortality among women globally, with early detection being critical for improving prognosis and survival rates. While mammography is widely used for screening, its limitations in young women and those with dense breast tissue have led to the increased use of ultrasound (US) imaging as a complementary tool. However, the quality of breast US images can vary significantly, with body mass index (BMI) emerging as a potential influencing factor. This study investigates the correlation between BMI and breast US image quality, focusing on its implications for breast carcinoma detection in Malaysian women. A prospective observational study was conducted in a hospital in Alor Setar, Kedah, involving 18 female patients with breast lesions classified as Bi-RADS 4 or above. Participants were categorized into normal (18.5–24.9 kg/m²), overweight (25–29.9 kg/m²), and obese (≥30 kg/m²) BMI groups. Breast US images were evaluated for pathology demonstration, spatial resolution, and contrast resolution using a subjective scoring survey assessed by five medical officers. Statistical analysis, including Spearman correlation and Cronbach’s Alpha coefficient, was performed to determine the relationship between BMI and image quality.The results revealed a weak negative correlation between higher BMI and inferior image quality, particularly in obese patients. However, the impact of BMI was not as significant as initially expected, with minimal disparities observed between normal and overweight groups. The normal BMI group achieved superior image quality, attributed to smaller breast volumes and optimal acoustic properties. Overweight patients demonstrated comparable image quality, likely due to adipose tissue acting as an acoustic interface. In contrast, obese patients exhibited the lowest image quality scores, primarily due to increased breast thickness and ultrasound wave attenuation. Despite these challenges, image quality in obese patients remained acceptable for clinical use. The study highlights that while BMI influences breast US image quality, other factors such as breast composition, lesion characteristics, and operator expertise play a more substantial role. Variability in breast tissue density and the skill of the sonographer were identified as critical determinants of image quality. These findings underscore the need for tailored imaging protocols and advanced technologies, such as high-frequency transducers and three-dimensional US, to optimize diagnostic accuracy across all BMI categories.